Lung Transplant
Lung Transplantation for Idiopathic Pulmonary Fibrosis
Lung transplantation is a surgery in which a person with severe, incurable lung disease receives either one healthy lung (single transplant) or two healthy lungs (double transplant) from a deceased donor. Lung transplantation can extend survival and improve quality of life for patients with advanced idiopathic pulmonary fibrosis (IPF) and some other interstitial lung diseases (ILD).1,2 This article discusses common questions about the process of evaluation for lung transplant, waiting for a donor, undergoing the procedure itself, recovery, long-term outcomes, and covering the costs.
When is time for me to consider lung transplant evaluation?
An evaluation is recommended if a person with ILD has started ambulatory oxygen therapy or has been hospitalized with an acute exacerbation (worsening) of the disease. It is also recommended if lung function is getting worse very quickly; for example, if the person’s percent predicted forced vital capacity drops by 10% or more in less than 6 months.3
That being said, there is no reason a person cannot be evaluated earlier in the disease course. Early referral for lung transplant evaluation can happen soon after diagnosis, and many doctors recommend this approach. A lung transplantation evaluation can take 6 months or more, so many doctors want to get their patients started as soon as possible. The International Society for Heart and Lung Transplantation also recommends early evaluation.3
Be aware that most transplant centers will not evaluate patients who are older than 70 to 75 years of age. This is because the likelihood of a successful transplant is low for patients who are above this age range.
Do I have to have a primary caregiver or caregivers set up before undergoing a lung transplant evaluation?
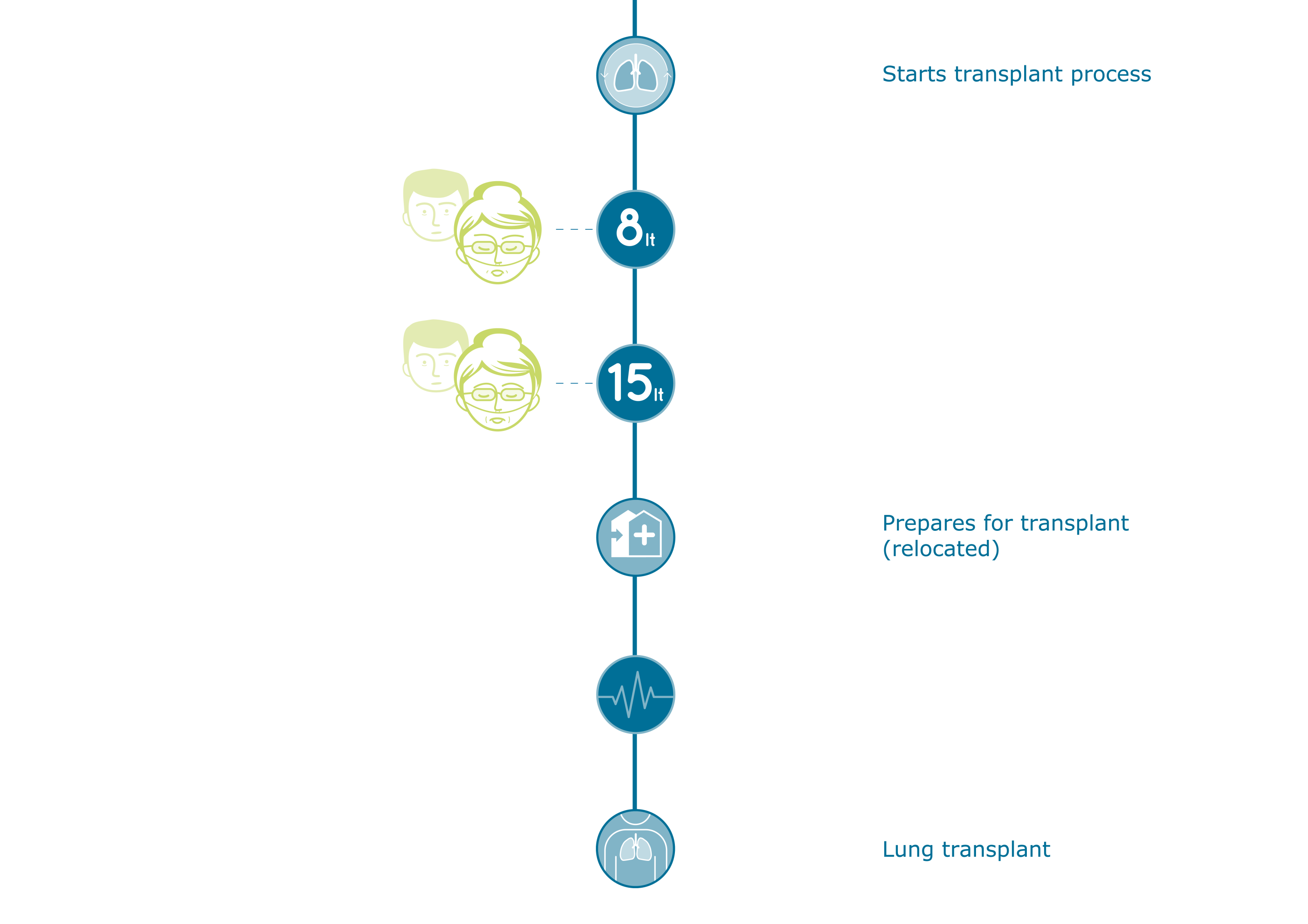
Yes. Transplant centers require you to have identified your primary caregiver or caregivers before the evaluation process begins, and the caregiver(s) must accompany you during the evaluation process. The primary caregiver is expected to attend appointments and education sessions; drive you to and from appointments; help you manage your medications after surgery; and provide personal care support, including with bathing, grocery shopping, cooking, and chores, after surgery. You will not be able to do these things reliably for yourself for weeks to months after surgery.
Transplant centers will not consider someone for placement on the transplant list if that person does not have a primary caregiver or caregivers who are fully committed to the necessary responsibilities. It is not possible to undergo lung transplantation “on your own”.4
What else must I do before a lung transplant evaluation?
Transplant centers often have many requirements that must be met before they will conduct a lung transplant evaluation. These may include4:
- Stop smoking and using nicotine products (patches, gum, vaping), illegal drugs, and alcohol. There may be a time requirement associated with this (e.g., no use at all in the past 6 months).
- Keep body weight in the healthy or mild-to-moderately overweight range. Patients with a body mass index that is in the obese range will often be required to lose weight before undergoing a lung transplant evaluation.
- Participate in pulmonary rehabilitation for a certain number of sessions.
- Take certain medications or undergo certain procedures to get other conditions under control (e.g., treatment for gastroesophageal reflux disease).
What is involved in a lung transplant evaluation?
The first step is for your pulmonologist to refer you to a transplant center for an evaluation. If there is more than one center in your area, you may wish to speak with the staff at each center to get a feel for the eligibility criteria, methodology, and culture of each. Many patients, however, do not have a choice among centers.
Each center conducts the evaluation process a little differently, but it will be a multi-day process that involves a great deal of testing. If you do not live within driving distance, you will need to stay in accommodations nearby the center.
During the evaluation, a number of different types of providers will meet with you. These may include:
- Transplant coordinator: This is usually a nurse who is specially trained in lung transplant care. The coordinator helps with scheduling appointments, interpreting test results, teaching you about lung transplantation, connecting you with resources (such as support groups, arrange for pulmonary rehabilitation, assist you with understanding and obtaining your medications, and providing education and support to your primary caregiver).
- Transplant pulmonologist: This is a medical doctor who specializes in lung disease. This provider will conduct a physical examination, review your current medications, assess the risks and benefits of transplant surgery, and make recommendations to the team.
- Transplant cardiologist: This is a medical doctor who specializes in heart disease. Having ILD can strain the heart, so this provider will perform a physical examination and tests for heart function and then make recommendations to the team.
- Transplant surgeon: This is a medical doctor who specializes in transplant surgery. This provider will complete a general surgical evaluation, review any previous procedures you have had, and assess the risks and benefits of transplant surgery. If you eventually undergo transplantation, this provider will perform the actual transplant surgery and will follow up with you after surgery.
- Insurance coordinator: This administrative professional will review your insurance coverage to ensure that you will not be put into financial hardship by the transplant process and all the required care.
- Social worker: This mental health professional will evaluate your social support network and psychological readiness for the transplant process. The social worker also provides support, referrals to outside support groups, and educational resources to the transplant patients and their families throughout the process.
What tests will be performed during the lung transplant evaluation?
Each center has its own list for testing. In general, tests will include most, if not all, of the following:
- Chest x-ray
- Pulmonary function tests
- 6-minute walk test
- Blood tests: These will include blood typing and tissue typing, which are needed to know how to match you to potential donors. Other blood tests will check your overall health, metabolism, kidney function, liver function, thyroid function, and immune function. Tests will also be done to check for a variety of diseases that might present a risk during a transplant (HIV, hepatitis, herpes, etc.).
- Ventilation perfusion scan: Contrast media is injected into a vein and then the lungs are scanned to detect the location of the contrast media as your blood circulates. This test provides information about the blood flow to your lungs and how much air each lung receives.
- High-resolution computed tomography (HRCT) scan: This imaging study provides information about the extent of fibrosis (scarring) in your lungs.
- Electrocardiogram: Electrodes are placed on your chest and back and the rhythm of your heart is recorded and checked for abnormalities.
- Echocardiogram: This is an ultrasound scan of the heart that allows the doctor to view the heart’s pumping action in real time.
- An echocardiogram is often combined with Doppler ultrasound to evaluate blood flow across the heart’s valves.
- Cardiac catheterization: During this test, a cardiologist inserts a long, slender tube (called a catheter) through a blood vessel in the groin or arm and into the heart. Contrast media is injected through the catheter and into the heart. As blood moves through the heart’s chambers, valves, and major vessels, an imaging scanner will track the movement of the contrast medica. This allows the doctor to identify blockages in your heart valves, check to see if coronary arteries are narrowed, and if the heart is pumping strongly enough.
- Esophageal manometry: A catheter is passed into your stomach through your nose. During the test, you will be asked to swallow water. This procedure shows your doctor how the muscles in your esophagus work when you swallow.
- 24-Hour gastric pH test: A catheter is passed into your stomach through your nose and will stay in place for 24 hours. You go about your normal activities during this time, and you will keep food and drink diary while the test is in progress. The catheter has sensors that record how often acid from your stomach comes up into your esophagus.
- Sigmoidoscopy or colonoscopy: A camera is passed through the anus into the colon to look for abnormalities or growths in the bowel.
- Bone densitometry: This type of imaging study, also called dual-energy x-ray absorptiometry, DEXA or DXA, uses a very small dose of ionizing radiation to produce pictures of the lower spine and hips. The scan quickly and accurately measures the density of bone. It can show if you have osteopenia or osteoporosis, diseases in which the bones’ mineral content and density are low, and the risk of fractures is high.
What happens after the lung transplant evaluation?
Once you have finished all the appointments and testing, the entire transplant team will meet and discuss your situation. They may decide that lung transplantation is not the best treatment option. This might be because of another condition (cancer, heart disease, etc.). It might be because of a lack of social support and caregivers. It might be because of lifestyle factors (smoking, drinking, obesity, etc.).
The team might also decide that you are a good candidate for transplant, but it is too soon in the disease process. They will continue to monitor your health and will move you to the transplant waiting list when it is the best time for you.
The team might decide that lung transplantation is the best treatment option for you now. You will be approved and put on the national United Network for Organ Sharing (UNOS) lung transplant waiting list and assigned a Lung Allocation Score (LAS).
Be aware that even if the lung transplant evaluation team feels you are a good candidate for transplantation now, the choice is up to you. You can decide to put your name of the UNOS lung transplant waiting list, or not. You are also always permitted to remove your name at any time from the transplant list if you change your mind.
What is the Lung Allocation Score (LAS)?
The Lung Allocation Score is assigned using criteria mandated by UNOS5. UNOS is a non-profit organization that is contracted by the US federal government to be the nation’s Organ Procurement and Transplantation Network (OPTN). The OPTN creates policies with the goal of making the best use of donated organs across the United States as a whole. Every transplant center must follow the policies.
An LAS is assigned to every person on the lung transplant list who is age 12 and older based on specific criteria (Figure 1). The lung allocation score estimates the severity of the person’s illness and the chance of success following a lung transplant. The score is a number from 0 to 100, and a number will receive higher priority for a lung offer when a compatible lung becomes available in the same geographic zone. However, note that lungs from pediatric (ages 0-11 years) and adolescent (ages 12-17 years) donors are offered first to pediatric and adolescent transplant candidates before they are offered to adults.5
Your LAS is updated every 6 months, which means you will need to undergo some repeated tests if you are on the list for more than 6 months.
How does donor matching work?
OPTN matches donors based on the following criteria6:
- Blood type
- Body size
- LAS
- The distance between the hospitals of the donor and transplant candidate
- Length of time on the waiting list
- Availability of the transplant candidate (must be able to arrive to the transplant center within 4 hours)
- The transplant candidate’s immediate health (e.g., if the person is battling an infection, they would not be transplanted)
- The condition of the donor lungs (how long they can remain suitable for transplant).
What if I don't live near a lung transplant center? Do I need to relocate if I am put on the lung transplant waiting list?
You will need to be able to arrive at the transplant center within 4 hours after getting the call that donor lungs are available. Some patients may choose to use a private charter flight to accomplish this if they live outside of driving distance. This is not affordable for many patients. Some organizations provide these types of flights for free or a reduced cost for transplant candidates. UNOS keeps a list of financial resources.7
What happens while I wait to receive the call that donor lungs are available?
Lung transplantation candidates on the waiting list are carefully monitored, and they continue to undergo treatment aimed at slowing the scarring in the lungs and improving physical function. These treatment options may include oxygen therapy, anti-fibrotic medication, pulmonary rehabilitation, and supportive care.8
If you have other conditions, these will be managed carefully as well. Conditions like GERD, heart disease, or swallowing disorders can impact transplant success, so active treatment is required. You will be encouraged to lose weight if needed, eat a nutritious diet, exercise under the guidance of your treatment team, and build up your social support network before transplantation.8
Mental health support for symptoms of anxiety and depression is important as well. These symptoms are nearly universal among patients with ILD on the transplant list at one time or another because the process is very stressful.9 Support may come from family and friends, patient support groups, a therapist, a member of the clergy, or other mental health support resources. The social worker at the transplant center can be very helpful for finding resources.
What happens when I get the call that donor lungs are available?
Each transplant center will have its own procedure that you will follow. In general, when you get the call, do not eat or drink anything. Carefully have your caregiver drive you to the hospital, or use whichever mode of transportation has been chosen in advance. Once there, you will undergo tests to ensure that you are not actively sick with an infection or have another problem that would prevent the surgery from happening. The lungs will be inspected and tested as well. Sometimes, either the person or the donor lungs are not suitable for transplant that day. This is extremely disappointing, but it does happen. It is important to prepare with your mental health support team for this possibility.4
If the surgery proceeds, it will last about six to 12 hours. You will then be transferred to the intensive care unit until you are stable enough to be in a regular hospital room. You will stay in the hospital for at least two to three weeks.4
What is life after transplant like?
Once home, you will need a caregiver with you 24 hours a day for the first several months after surgery. You will have very frequent appointments with your transplant team and will need someone to drive you there. You will have many medications that you will need to take to prevent infection and to prevent your body from rejecting your new lungs.4
At first, your caregivers will need to do most personal and household tasks together with you or will need to do them for you. You will need to gradually build up strength to perform activities of daily living such as bathing, dressing, cooking, etc., over the first few weeks. You will not be able to drive for at least six weeks. You will not be able to return to work for at least two months. You will not be able to lift more than 5 pounds for at least six months.4
You will be expected to return to physical activity, and may be required to attend rehabilitation sessions. Your team will encourage you to slowly build up your ability to exercise. You will start with stretching and short walks. Contact sports will need to be permanently avoided to prevent injury to your new lungs.4
The biggest risk after transplant is infection. You will need to avoid crowds and sick people, wear a mask when in public, wash your hands frequently, and receive all recommended vaccines.4,8
Smoking and tobacco products must be completely avoided for life. You will need to avoid secondhand smoke as well.4,8
What are the chances of survival?
The most recent data from the International Society for Heart and Lung Transplantation Registry’s quarterly report includes survival rates for transplants performed between January 1, 2013, and December 31, 2016. The report stated that 87.5% of patients with idiopathic interstitial pneumonia who were transplanted in North America in that time were still alive at one year post-transplant. At three years post-transplant, the survival rate was 69.1%.10
How much does the whole thing cost, and how is it covered?
Lung transplantation is extremely expensive.11 Costs include:
- Lung transplant evaluation
- Ongoing management by the evaluation team
- Lung transplantation surgery
- Hospital stays
- Pulmonary rehabilitation
- Medications necessary to protect you from infection and from rejecting the new lungs (as high as $9,000 per month for the rest of your life)
- Durable medical equipment (e.g., a home spirometer to monitor lung function)
- Lost time from work for you and your caregivers
- Childcare costs
- Transportation and parking
- Lodging and meals.
- Hired help around the home during recovery (home health aides, yard work, cleaning, shopping, cooking, etc.).
In all, total costs can rise to hundreds of thousands of dollars, and in some cases, over a million dollars.
The financial/insurance coordinator at your transplant center will spend a great deal of time going over the financial implications with you and your caregivers before you are listed on the transplant waiting list. You will likely also need to speak with your insurance company directly to ask questions about coverage, the need for referrals, and out-of-pocket costs (co-pays, deductibles, medications that are not covered, etc.). The financial/insurance coordinator at your transplant center will walk you through the process.
Most insurance companies, including Medicare, provide some degree of coverage for the costs associated with lung transplantation. However, most patients cannot afford the co-pays and out-of-pocket costs even with insurance. For example, Medicare part B will only cover 80% of the costs of outpatient care; the remaining 20% is your responsibility. This out-of-pocket cost alone is often too much for one family to afford. Sometimes taking out a supplemental insurance policy is needed. In other cases, there may be financial support resources available through local, regional, or national organizations. Some patients with lower income and assets may be eligible for Medicaid. The social worker at your transplant center can help you determine if you are eligible for aid and help connect you with helpful resources.11
Unfortunately, even with insurance, most people who undergo lung transplantation find they need to do some degree of fundraising from friends, family, the local community, and charitable organizations to afford all the costs. Helpful guidance on financial assistance can be found in the UNOS list of financial resources7 and in the UNOS quick reference on covering the cost of transplant.
One very important thing to note: if your insurance plan changes or may change, contact the financial/insurance coordinator at your transplant center immediately to discuss this. Some common reasons that insurance might change include:
- Loss of your employment
- Loss of your spouse or partner’s employment
- Aging out of a parent’s insurance plan
- Divorce or separation from a spouse who is the insurance policy holder
- Retirement
- Enrollment in Medicare
It is important to keep on top of insurance and financial issues because you can be placed on hold on the transplant waiting list if your financial coverage is insufficient or if your coverage lapses for a time.11
References and Further Reading
- Thabut G, Mal H, Castier Y, et al. Survival benefit of lung transplantation for patients with idiopathic pulmonary fibrosis. J Thorac Cardiovasc Surg. 2003;126(2):469-475.
- Bleisch B, Schuurmans MM, Klaghofer R, et al. Health-related quality of life and stress-related post-transplant trajectories of lung transplant recipients: a three-year follow-up of the Swiss Transplant Cohort Study. Swiss Med Wkly. 2019;149(07-08):10.4414/smw.2019.20019.
- Weill D, Benden C, Corris PA, et al. A consensus document for the selection of lung transplant candidates: 2014--an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2015;34(1):1-15.
- Pulmonary Fibrosis Foundation. Lung Transplantation.
- United Network for Organ Sharing. Questions and Answers for Transplant Candidates about Lung Allocation.
- United States Health Resources & Services Administration. Matching Donors and Recipients.
- United Network for Organ Sharing. Transplant Living: Financial Resources Directory.
- Kapnadak SG, Raghu G. Lung transplantation for interstitial lung disease. Eur Respir Rev. 2021;30:210017.
- Skogeland U, de Monestrol I, Godskesen TE. Experiences of individuals awaiting lung transplantation. Respir Care. 2018;63(12):1535-1540.
- The International Society for Heart and Lung Transplantation. International Thoracic Organ Transplant Registry Quarterly Data Reports: North America. Accessed September 16, 2021.
- United Network for Organ Sharing. Transplant Living: Covering Transplant Costs.