Palliative Care

Supportive Care for Patients with Interstitial Lung Disease
Bothersome cough that exhausts you during the day and keeps you up at night. Fatigue that makes it hard to accomplish daily life tasks or to socialize. Breathlessness that makes you feel anxious, worried, or even, at times, trapped.
For many people with ILD, the symptoms are difficult to bear. You are not alone in feeling this way. In addition, a lack of information about what is happening and what to expect just adds to the worry and exhaustion. Social isolation, depression, panic attacks, and anxiety are often the result for people living with ILD, and for their caregivers as well.1,2
With all of these challenges, good supportive care is essential. Supportive care can improve bothersome symptoms and improve daily quality of life. It can provide education, answers, and practical advice to patients and caregivers. It can help build up hope and provide social support. Good supportive care takes into account the whole person – mental, physical, emotional, social, and practical.
The good news is that supportive care is available to most people with ILD and their caregivers. It is called palliative care.
The name “palliative care” causes a lot of anxiety and confusion for many patients and caregivers. The name comes from the word “palliate”, which means “to cloak, cover, ease, or reduce the burden”. Palliative care is not the same as “end-of-life” care, is not the same as hospice care, and does not mean a patient is “about to die”. Palliative care does not mean that you must stop taking mediations or treatments that aim to prolong life or treat your disease. It does not mean the doctor has given up on you. In fact, many patients who receive good palliative care along with specific treatments for their disease end up living longer than those who receive specific treatments for their disease only.3
This article will describe how palliative care works and offer information about how palliative care can be helpful for patients, families, and caregivers at every stage of the ILD journey.
“We need to take the stigma away from the words ‘palliative care’ and disassociate it from hospice care. The reality is, at this point in time, there is no cure for IPF. The way I see it, patient care is best focused on the most and best support immediately after diagnosis, because the patient’s best time is directly in front of them.”
— Judy, living with idiopathic pulmonary fibrosis and receiving palliative care
What is palliative care?
Palliative care is supportive care with four goals:
- Help a person live as well as possible for as long as possible in a way that fits with that person’s values and goals.
- Prevent and reduce suffering (physical, emotional, and social).
- When the time eventually comes, help a person achieve the end-of-life experience that fits with the person’s values and priorities.
- Support and relieve the suffering of caregivers.
People with ILD can receive palliative care alongside disease-specific treatments like anti-fibrotic medications, oxygen supplementation, and pulmonary rehabilitation. You do not have to give up treating your disease to get good supportive care. 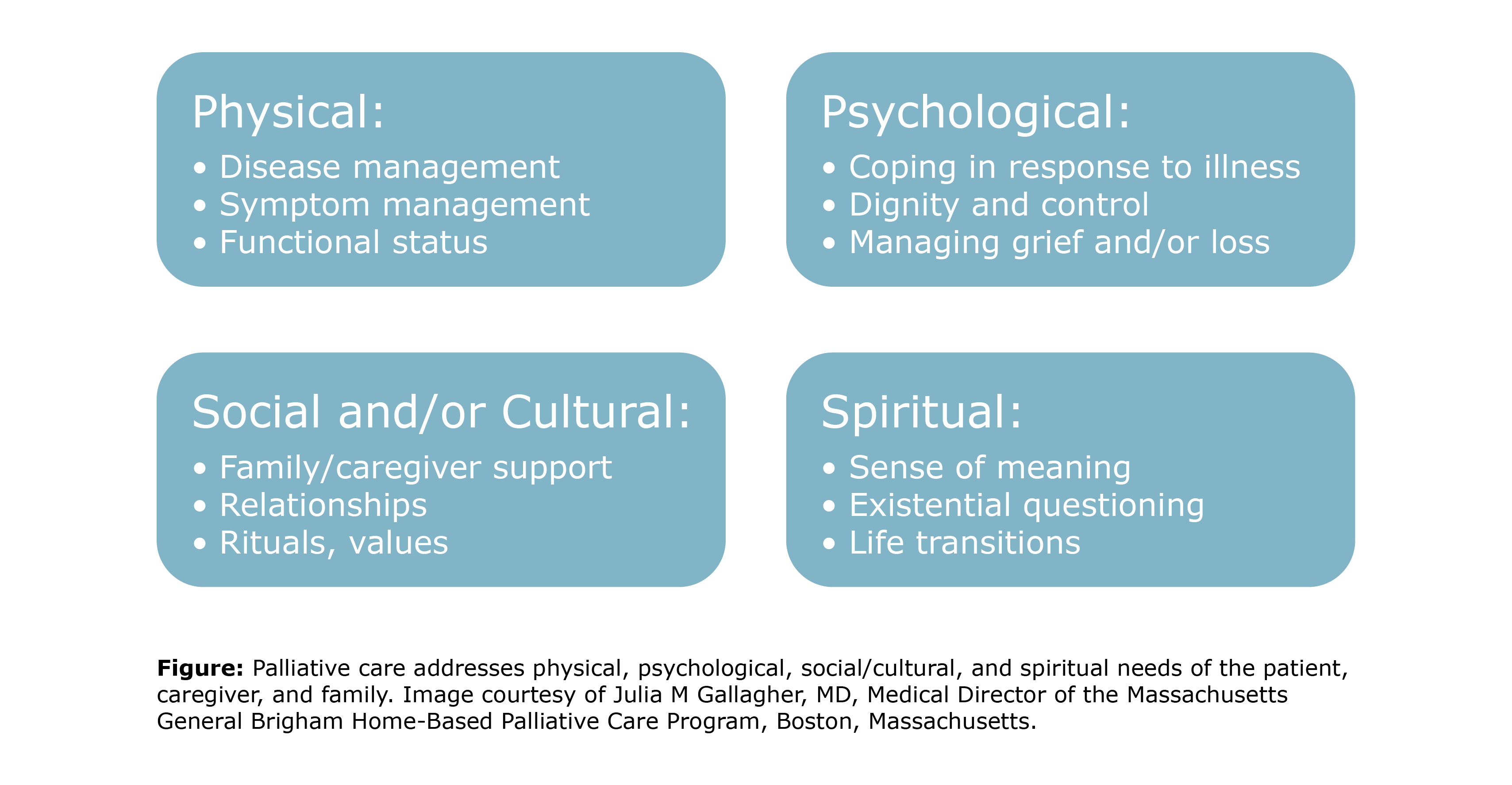 Who provides palliative care and what is provided?
Who provides palliative care and what is provided?
Care is provided by an interdisciplinary team that includes:
- Palliative care doctors
- Palliative care nurse practitioners
- Palliative care nurses
- Palliative care social workers.
Your physician may also prescribe the services of physical therapists or occupational therapists.
This interdisciplinary care team can assist patients and caregivers in the following ways:
- Palliative care clinicians can assess the need for medications and make recommendations for medications or non-medication options to relieve or reduce symptoms.
- Physical and occupational therapists can recommend durable medical equipment to make activities of daily life easier. They can also help patients learn ways to conserve energy during daily activities.
- Social workers can help manage the stress of living with ILD and help identify and link patients and families to helpful community resources. Social workers can also link patients and families to spiritual support resources, if desired.
Palliative care can be provided in hospitals, long-term care facilities, or at home.
Why are caregivers included in palliative care?
The palliative care team supports caregivers as well as patients. Caregivers are included because they can become stressed and overwhelmed, putting them at increased risk for illness, depression, anxiety, and social isolation. A key part of palliative care is providing education and social/emotional support to caregivers.4
Is palliative care another name for hospice?
No. Palliative care is not the same as hospice care. Palliative care is specialized, supportive medical care delivered by a multidisciplinary team of healthcare professionals. Hospice care is an insurance benefit provided for a person with a terminal illness whose doctor believes he or she has 6 months or less to live if the illness runs its natural course. When entering hospice care, patients confirm with their insurance company that they would like palliative care only, rather than also having direct treatments for ILD that might prolong life.5
Hospice care allows patients to choose to avoid more hospitalizations and medical interventions. It is usually provided in the patient’s residence (home, assisted living facility, or long-term care facility). Choosing to enroll in hospice care is voluntary. If a person enters hospice care and then decides to return to direct treatment for ILD and leave hospice, that is always allowed.
Is palliative care another name for home health care?
No. Home health care is an insurance benefit with the goal of treating the underlying illness or injury.6 Usually, this health care is provided by skilled nurses, physical therapists, and occupational therapists. Home health care can be used for a short time, such as recovery from a surgery, or a long time, such as with a person who has had a stroke.
The team will work to help the patient get better, regain their independence, and become as self-sufficient as possible. Improving the quality of life for the patient and caregiver and providing social/emotional support may happen, but the focus of home health care is generally on rehabilitation and recovery.
What are the benefits of palliative care for people with ILD?
On average, people with ILD experience more difficulties because of their condition than people with lung cancer do.1 People with ILD have a higher burden of symptoms, worse quality of life, more difficulty with day-to-day activities, and more social isolation than are reported by people with cancer. These difficulties also last longer.7
Living with ILD can be very challenging. Taking care of a loved one with ILD can be very challenging. The supportive (palliative) care team is there to help. Benefits include increased comfort, less anxiety and depression, less social isolation, increased understanding of the disease and how to cope, increased ability to do the things you enjoy doing, and better overall quality of life.8,9
When is the best time to start palliative care in the ILD journey?
Palliative care is always a good option to discuss. In an ideal world, it would begin as soon as the person is diagnosed. If that is not possible or desired, then it is useful to consider and discuss palliative care if hospitalizations increase, medications are no longer working well, or supplementary oxygen is prescribed.
Unfortunately, many doctors do not bring up this issue with patients because patients often misunderstand. They may believe palliative care and hospice are the same, and that their doctor is “giving up”. The doctor may avoid the topic because of worry about taking away hope or sending the wrong message about continuing your treatment to prolong life. But if you bring it up with your doctor, most doctors are happy to refer you to the palliative care team.
In a survey study of 69 healthcare professionals who treat patients with ILD, respondents were asked to explain at which point in the disease course they initiate palliative care for their patients. Around a third of respondents answered that palliative care was started at an early stage of the disease if desired by patients. Most reported that palliative care was initiated in more advanced stages of the disease. Unfortunately, 20% of respondents stated that palliative care was only initiated at the end of life.10 The message is: feel free to speak up with your doctor about this topic.
Does Medicare cover palliative care?
Yes, with some rules that are important to understand.
Medicare Part B (medical insurance) will usually help cover the cost of seeing a palliative care doctor or nurse practitioner. It will also cover medically necessary services and supplies, mental health care, and durable medical equipment. Many of these services and supplies will be covered along with coverage for treatments that directly address your disease with the intent to prolong your life. Home health aide services and respite care will not usually be covered.
Medicare Part D (prescription drug insurance) will cover prescription drugs, including those a person needs when receiving palliative care. These may include medications for anxiety, pain relief, nausea, fatigue, or other symptoms. The copayment for these will be the standard rate for Medicare Part D.
If you have Medicare coverage through a Medicare Advantage plan, you will have at least the same benefits as original Medicare. Some Medicare Advantage plans include additional coverage. You will need to call your plan manager directly to ask what will be covered.
Do I have to be “homebound” to receive palliative care services?
This is a complicated question to answer. First, let’s consider the definition of homebound. “Homebound” (according to insurance companies) refers to a person who needs the aid of supportive devices, or special transportation, or the assistance of another person in order to leave the home OR has a condition such that leaving the home is medically contraindicated (not recommended). In addition, the person must generally be unable to leave the home without “considerable and taxing effort”.6
Insurance will generally cover palliative care services and does not require a patient to be homebound to do so. In contrast, some insurance companies (including Medicare), require a person to be homebound to cover the services of home health care providers.
The difficulty arises when an agency provides both palliative care services and home health services. Some of their healthcare providers (usually social workers, physical therapists, and occupational therapists) will be enrolled with the private insurance companies and Medicare in a way that only allows them to bill for home health services (meaning, patients must be homebound). This causes billing difficulty when patients receive palliative care from those same healthcare providers through the agency.
Here’s an example. Let’s say a patient is receiving palliative care, but is not homebound. The agency sends out a physical therapist to this patient’s home to provide supportive care. However, the physical therapist is enrolled with insurance companies only as a home health care provider. Since the patient is not homebound, insurance will not cover this visit.
This problem is why some agencies that provide palliative care tell patients they must be homebound to receive palliative care. This is not true. The truth is that the agency’s care providers are enrolled with insurance companies in a way that they can only receive payment as home health care providers. The agency is making the billing process simple for itself by requiring all enrolled patients to be homebound.
The solution to this problem is to be very clear with any agency you call when you ask about palliative care services. For example, you can call and explain, “I would like palliative care, but I am not homebound. Are all the providers you send to my home for palliative care able to bill my insurance in a way that will be covered? Does this include social workers, physical therapists, and occupational therapists?”
There are agencies that can send a team of healthcare providers who can provide palliative care services and can also bill insurance without you being homebound. You may need to call several agencies. You can also ask members of your ILD healthcare team for guidance in this process.
How can I find information about palliative care services in my area?
One of the best ways is to bring the topic up with your doctor, nurse, or social worker. Feel free to speak up about your wish to try palliative care alongside any of your direct treatments for ILD. Your healthcare team may hesitate to bring it up, but will likely be happy to explore this option with you when you bring it up.
Other resources include:
- The Hospice and Palliative Care Federation of Massachusetts Palliative Care Directory.
- The Center to Advance Palliative Care Provider Directory.
- The National Hospice and Palliative Care Organization Care Provider Directory.
Further Reading
National Institute of Nursing Research. Palliative Care: The Relief You Need When You Have a Serious Illness.
US National Library of Medicine Medline Plus. Palliative Care.
References
- Wysham NG, Cox CE, Wolf SP, Kamal AH. Symptom burden of chronic lung disease compared with lung cancer at time of referral for palliative care consultation. Ann Am Thorac Soc. 2015;12(9):1294-1301.
- Carvajalino S, Reigada C, Johnson MJ, Dzingina M, Bajwah S. Symptom prevalence of patients with fibrotic interstitial lung disease: a systematic literature review. BMC Pulm Med. 2018;18(1):78.
- Higginson IJ, Bausewein C, Reilly CC, et al. An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: a randomised controlled trial. Lancet Respir Med. 2014;2(12):979-987. doi:10.1016/S2213-2600(14)70226-7
- van Manen MJ, Kreuter M, van den Blink B, et al. What patients with pulmonary fibrosis and their partners think: a live, educative survey in the Netherlands and Germany. ERJ Open Res. 2017;3(1):00065-2016.
- Medicare.gov. Hospice Care.
- Medicare.gov. Home Health Services.
- Barratt SL, Morales M, Spiers T, et al. Specialist palliative care, psychology, interstitial lung disease (ILD) multidisciplinary team meeting: a novel model to address palliative care needs. BMJ Open Respir Res. 2018;5(1):e000360.
- Zou RH, Kass DJ, Gibson KF, Lindell KO. The role of palliative care in reducing symptoms and improving quality of life for patients with idiopathic pulmonary fibrosis: a review. Pulm Ther. 2020;6(1):35-46.
- Wijsenbeek MS, Holland AE, Swigris JJ, Renzoni EA. Comprehensive supportive care for patients with fibrosing interstitial lung disease. Am J Respir Crit Care Med. 2019;200(2):152-159.
- Moor CC, Wijsenbeek MS, Balestro E, et al. Gaps in care of patients living with pulmonary fibrosis: a joint patient and expert statement on the results of a Europe-wide survey. ERJ Open Res. 2019;5(4):00124-2019.