A Primer on Vaccines
Vaccine Basics: Essential Information in the Time of COVID-19
The story of vaccines begins with smallpox, which was reported in ancient Egypt, China, and India as early as 400 BCE (Before Common Era). This devastating disease was caused by the variola virus. Symptoms included high fever, sores in the mouth and throat, and pus-filled blisters erupting all over the face and body. It killed about 3 in 10 people who contracted it. Those who survived were often left with heavy scarring, and some went blind from the disease. Thankfully, smallpox has been eradicated from the world since 1980, thanks to vaccination.
Although people in earlier times in history did not understand that smallpox was caused by a virus, they understood that people who contracted smallpox and survived never contracted it again. In 1796, an English doctor named Edward Jenner observed something interesting about cowpox, a disease which was not fatal to humans and which was often seen in milkmaids at the time. He observed that milkmaids who had contracted cowpox did not contract smallpox during smallpox outbreaks. He suggested that immunity to cowpox was also giving the milkmaids immunity to smallpox. Though he did not know why, his theory was correct. The cowpox virus and the smallpox virus are very closely related, so immunity to one provides protection from the other.
Jenner conducted an experiment to test this theory by taking puss from a milkmaid’s cowpox blister and scratching it into the arm of a 9-year-old boy. The boy did not become sick from this tiny bit of cowpox puss. Months later, Jenner exposed the boy a number of times to the variola virus (smallpox virus), but the boy never became sick with smallpox. While such unethical experiments would never be allowed today, they were the scientific basis for the modern vaccination program that successfully rid the world of smallpox less than 200 years later.
The Goal of Vaccination
As described in the Immunology Primer, the immune system keeps a memory of many of the different types of pathogens that it encounters by creating memory B and memory T cells. Memory cells live for many years, or in some cases a person’s entire lifetime. When memory cells encounter their target pathogen again, they immediately mount a defense. Often the response is so quick and so strong that the person never even knows they are fighting off a repeat invasion from a pathogen they overcame before. They do not feel sick at all.
The goal of vaccination is to present the immune system with a killed, weakened, or partial pathogen so that immune cells will respond and eventually make memory cells. Those memory cells will provide protection if the person is exposed to the actual, active pathogen later in life. The trick is to make sure that the vaccine itself does not actually cause illness in the person who is vaccinated.
One useful tool that researchers have developed is to inject adjuvants along with the vaccine. An adjuvant is a substance (such as alum) that can provoke a stronger response from the immune system than would happen with the vaccine alone. It is risky to make a vaccine that is too similar to an active pathogen, so researchers purposely make the vaccine weak and not capable of causing illness. An adjuvant can ramp up the immune response to the vaccine without putting the vaccinated person at risk of actual illness. Not all vaccines use adjuvants, but many do.
Vaccine Platforms
How can scientists create a vaccine that is just enough like the active, dangerous pathogen to prompt the immune system to make protective memory cells without actually causing illness? Over the years, there have been many ideas of how to meet this challenge. These different ideas, or approaches, are called vaccine platforms.
The first type of vaccine platforms are classical vaccine platforms, which have been around for over a hundred years. These vaccines contain actual pathogens or toxins that have been weakened or killed. There are a number of approved vaccines that are based on the classical vaccine platforms. They have known safety records, and the pros and cons are well understood.
There are also newer platforms that have been developed over the past several decades. These can be divided into conventional vaccine platforms and next-generation vaccine platforms.
Conventional vaccine platforms do not contain actual pathogens. They contain parts of the pathogen that can provoke an immune response. These parts are known as antigens.
Next-generation platforms do not use pathogens or antigens. Instead, they use genetic material taken from pathogens. Our own body cells can take up the genetic material and make pathogen proteins from it. These proteins act as antigens, provoking an immune response.
Below is a detailed description of each type of vaccine platform that is in active use or development in 2020.
Classical Vaccine Platforms
Live-attenuated vaccines are made by taking a pathogen that causes disease in humans and weakening it. Pathogens can be weakened in several ways. Usually, the pathogen is injected into cell cultures or chick embryos in the laboratory. The pathogen is allowed to grow, and then is collected and injected into new cell cultures or chick embryos. This is called a passage, and it is repeated dozens or hundreds of times. With each passage, the pathogen becomes better at growing and infecting cells in culture or in chick embryos, but loses its ability to grow in and infect human cells. When the weakened pathogen is injected into a person as a vaccine, it will be unable to cause illness. However, the pathogen will still provoke an immune response. These will protect against any later infection with the disease-causing version of the pathogen.
Inactivated vaccines are created by applying heat or chemicals, such as formaldehyde or formalin, to pathogens that cause disease in humans. The heat or chemicals destroy the ability of the pathogens to grow and infect human cells. However, the structure of the pathogen remains the same, and it produces an immune response when injected into humans. One downside is that inactivated vaccines do not produce as strong of an immune response as live-attenuated vaccines. Often multiple doses of the vaccine are needed, or sometimes “booster” shots are given every few years. Adjuvants are often given along with the vaccine to increase the immune response.
Toxoid vaccines are made from toxins produced by bacteria. For example, tetanus is caused by a chemical toxin made by a type of bacteria, rather than directly by the bacteria themselves. To make a vaccine, the toxins are inactivated using heat or chemicals, leaving the structure of the toxin intact. Toxoid vaccines work similarly to inactivated pathogen vaccines. When the inactivated toxin vaccine is injected into humans, it provokes an immune response. Adjuvants are often given along with the vaccine to increase the immune response.
Conventional Vaccine Platforms
Subunit vaccines contain only parts of a pathogen, not the entire pathogen. Researchers must invest time into carefully studying the structure of the pathogen to figure out which fragments (or antigens) from the pathogen can produce an immune response. The immune response must be strong enough to produce memory B and T cells that can protect against a future infection with the whole, active pathogen. Candidate antigens are tested in cell cultures in the laboratory, and then in animal models, before being tested in humans. The antigens used in subunit vaccines are sometimes proteins and sometimes complex sugars called polysaccharides. Sometimes these antigens are chemically attached (conjugated) to a substance that can produce a stronger immune response, such as inactivated tetanus toxin. When attached in this way, the vaccine is called a conjugate vaccine. Subunit vaccines are very safe and can be given to people with compromised immune systems. They produce a weaker immune response on their own than live-attenuated vaccines, so they usually require multiple doses or “booster shots” and an adjuvant to boost the immune response.
Virus-like particle vaccines work to protect against certain diseases caused by viruses. Virus-like particles are made up of the outer structure of the virus, but with no genetic information contained inside. Without the genetic information, the virus-like particle cannot infect cells or cause disease. Virus-like particles are made by injecting viral genetic material into cells in the laboratory (usually hamster cells or yeast cells). The cells allow the viral proteins to be assembled into particles. Large amounts of these cells are grown in the laboratory, and then the virus-like particles are collected and purified. These types of vaccines can produce a very strong immune response, similar to live-attenuated pathogen vaccines, but are very safe. It is impossible for any real infection to happen. The downside is that virus-like particle vaccines are difficult to design and make, and not all viruses have the type of structure that is suitable for a virus-like particle vaccine.
Antigen presenting cell vaccines are made with artificial cells that are grown in the laboratory. Normally, antigen presenting cells are a type of immune cell whose job it is to take up any antigens or pathogens they find in the body. These are broken down inside the antigen presenting cell. The resulting protein fragments (antigens) are displayed on the outside of the antigen presenting cell. Other immune cells see the antigens and sound the alarm, and an immune response is triggered. In antigen presenting cell vaccines, artificial cells are designed to display pathogen fragments on their surfaces. Once these artificial cells are injected into a person, that person’s own immune cells with recognize the “non-self” fragments (antigens) on the antigen presenting cells. This will trigger a strong immune response. The downside to this type of vaccine is that it is difficult to make and requires refrigeration, so worldwide distribution is impractical.
Next-Generation Vaccine Platforms
RNA and DNA vaccines use genetic material, either DNA or RNA, from pathogens. DNA can often be used on its own, because it is relatively stable and does not fall apart easily. RNA is much more unstable and tends to fall apart easily. Sometimes, RNA for vaccines is packaged into tiny spheres made of fat molecules (called lipid nanoparticles) for added stability. A bonus to lipid nanoparticles is that they can function as an adjuvant as well, increasing the immune response. After the genetic material is injected as a vaccine, cells in the body take it up. Our cells naturally have machinery inside them that takes the genetic material and uses it to make pathogen proteins (antigens). The proteins are then displayed on the outside of the cell. Immune cells see the pathogen proteins and react as though the cell has been “infected” by an active, dangerous pathogen. The immune cells sound the alarm, and an immune response is triggered against the pathogen proteins. The benefit of RNA and DNA vaccines is that they are easy to produce in the laboratory. The downside is that the safety of this type of vaccine has not been tested over the long term.
Viral vector vaccines are made when scientists take a common cold virus (adenovirus) or other weakened virus and remove the genetic material. This genetic material is replaced by some of the genetic material from another virus – the virus that the vaccine is targeted against. The new, hybrid virus cannot cause disease, but can get inside human cells. Once inside cells, the genetic material in the hybrid virus instructs the cells to make proteins, and those proteins are displayed on the surface of the cells. Other immune cells recognize these proteins as “non-self” antigens, so they trigger an immune response directed toward those antigens. Benefits of viral vector vaccines are that they are easy to make in the laboratory and do not need refrigeration. There are a number of downsides, however. First, there are limited safety data available. In addition, some percentage of the population has antibodies against various cold viruses. This type of vaccine may not work well in a person who has those antibodies. Another downside is that the dose of these types of vaccines must be kept low, because otherwise the immune response could become too strong and cause harm to the person receiving the vaccine. This creates the need for multiple doses or “booster shots”. 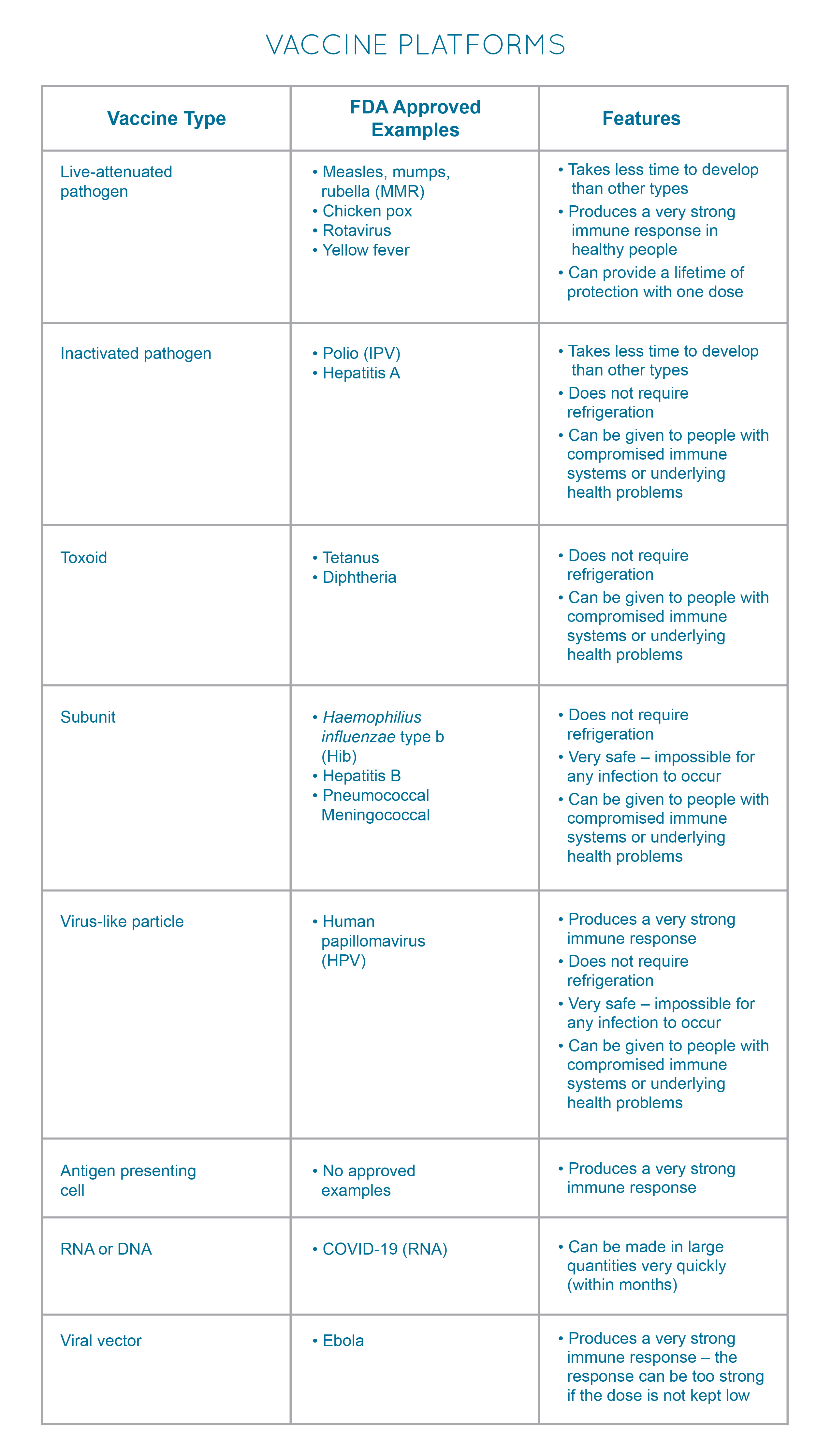 Herd Immunity
Herd Immunity
The eventual goal of vaccination programs within a country and across the world is to achieve herd immunity. This occurs when a large percentage of the people in a community, country, or the world are immune to a particular disease. Pathogens must spread by traveling from one person to another person, and they cannot do this when most people are immune to that pathogen. Even if a few people are still susceptible, the pathogen has a hard time “finding” them.
The specific percentage of people that must be immune to a pathogen to reach herd immunity is different for different pathogens. Very contagious pathogens, like the measles virus, can only be prevented from spreading in the community when 94% of people in that community are immune. For the polio virus, the threshold is 80%.
Herd immunity can be achieved by allowing a pathogen to spread rapidly in a population, and allowing most people to get the disease and recover. The obvious problem with this approach is that some pathogens cause a high death rate. Therefore, many people would have to die before heard immunity would be reached.
The other approach to herd immunity is a vaccination program where most of the population of a community, country, or the world receives a vaccine and gains immunity. This only works if the majority of people receive the vaccine. That is why vaccination is so important to eliminating the spread of illnesses like measles, influenza, and eventually COVID-19.
— Jillian Lokere and Aliaa Barakat
Glossary
Adjuvant: a substance (such as alum) that can provoke a stronger response from the immune system than would happen with the vaccine alone.
Antigens: Any substances that the immune system recognizes as “non-self” and which cause the immune system to respond. These may be proteins, certain types of sugars, or fragments of genetic material that are caused by pathogens invading the body.
Antigen presenting cells: Immune cells that circulate throughout the body and ingest (take up) pathogens, toxins, and any other substances that might be antigens. Fragments of these are then displayed on the outside of the antigen presenting cell. If other immune cells see the antigens and recognize them as “non-self”, they sound the alarm that an infection is underway, and an immune response is triggered.
Conjugate vaccine: A type of subunit vaccine in which an antigen is chemically attached to a larger substance that can trigger an immune response, such as a weakened form of tetanus toxin.
Herd immunity: Occurs when a large percentage of the people in a community, country, or the world are immune to a particular disease. Pathogens must spread by traveling from one person to another person, and they cannot do this when most people are immune to that pathogen. Even if a few people are still susceptible, the pathogen has a hard time “finding” them.
Lipid nanoparticles: Tiny spheres made of fat molecules. RNA and DNA from pathogens are placed inside these spheres to give them stability when they are used in vaccines.
Memory cells: These immune cells circulate throughout the body at low levels for many years, or in some cases a person’s entire lifetime, just waiting for their target pathogen to try to invade again. The minute memory cells recognize their old foe, they mount a defense. They provide long-term protection against pathogens that the body has fought off before.
Passage: A method for weakening a pathogen that will be used in a vaccine. Usually, the pathogen is injected into cell cultures or chick embryos in the laboratory. The pathogen is allowed to grow, and then is collected and injected into new cell cultures or chick embryos. This process is repeated dozens or hundreds of times
Pathogens: Harmful bacteria, viruses, fungi, parasites, and other microbes that can cause illness.
Polysaccharides: Complex sugar molecules that can act as antigens. Some vaccines use polysaccharides.
Vaccine platforms: Different ideas, or approaches, to creating vaccines that can provoke an immune response to a pathogen without actually making the vaccinated person sick. Classical vaccine platforms have been around for decades and have known safety records. Next-generation vaccine platforms that have only been developed over the last few years. Many next-generation platforms have not yet been used to make an approved vaccine; rather, they are still in the development stage.
References
- Centers for Disease Control and Prevention. Adjuvants and Vaccines.
- Centers for Disease Control and Prevention. Principles of Vaccination.
- Centers for Disease Control and Prevention. Smallpox.
- National Institute of Allergy and Infectious Diseases. Vaccine Adjuvants.
- University of Cambridge. RNA Vaccines: An Introduction.
- van Riel D, de Wit E. Next-generation vaccine platforms for COVID-19. Nature Materials. 2020;19(8):810-812.
- World Health Organization. Types of Vaccine and Adverse Reactions. Vaccine Safety Basics E-learning Course.